EVALUATING THE EFFICACY OF STATINS, ASPIRIN, AND ANTIHYPERTENSIVE THERAPY IN PREVENTING RECURRENT CARDIOVASCULAR EVENTS IN POST-MYOCARDIAL INFARCTION PATIENTS: A META-ANALYSIS
DOI:
https://doi.org/10.71000/ijhr155Keywords:
Aspirin, Cardiovascular Outcomes, Myocardial Infarction, Pharmacologic , Pharmacologic Therapy, Statins, Secondary Prevention, Systematic Review, Meta-analysisAbstract
Background: Myocardial infarction (MI) remains a leading cause of global morbidity and mortality, significantly burdening healthcare systems. Post-MI patients face a heightened risk of recurrent cardiovascular events, necessitating effective secondary prevention strategies. Pharmacologic interventions, including statins, aspirin, and antihypertensive therapies, are widely employed, yet their comparative efficacy is debated. This meta-analysis evaluates the effectiveness of these treatments in reducing recurrent cardiovascular events, aiming to inform optimized management strategies for this high-risk population.
Objective: To assess and compare the efficacy of statins, aspirin, and antihypertensive therapies in preventing recurrent cardiovascular events among post-MI patients.
Methods: This meta-analysis adhered to PRISMA guidelines and included studies published between September 25 and October 27, 2024. A systematic literature search was conducted in PubMed, Scopus, and Google Scholar using MeSH terms and keywords such as "statins," "aspirin," "antihypertensive therapy," "myocardial infarction," and "cardiovascular outcomes." Inclusion criteria required original studies evaluating the effects of these therapies on post-MI cardiovascular outcomes. Data on study characteristics, demographics, interventions, and outcomes were extracted. A random-effects model was applied for pooled analysis, with results presented as odds ratios (ORs) or hazard ratios (HRs) and mean differences (MDs) alongside 95% confidence intervals (CIs). Heterogeneity was assessed using the I² statistic, with sensitivity analyses performed to evaluate result robustness.
Results: Nine studies were included, encompassing 3,950 patients. High/moderate-intensity rosuvastatin reduced adverse cardiovascular events with an OR of 1.85 (95% CI: 1.65–2.10). Aspirin therapy demonstrated a 25% reduction in recurrent cardiovascular events among high-risk patients. Beta-blockers improved survival post-MI with an HR of 2.05 (95% CI: 1.85–2.30), and ACE inhibitors combined with canrenoate showed significant reductions in systolic and diastolic dysfunction, with an OR of 1.95 (95% CI: 1.70–2.20). Combination therapies of zofenopril and amlodipine yielded an OR of 1.75 (95% CI: 1.55–1.95). Overall heterogeneity was high (Q = 152.77, I² = 86.3%), reflecting differences in study designs and patient characteristics.
Conclusion: This meta-analysis highlights the efficacy of statins, aspirin, and antihypertensive therapies in reducing recurrent cardiovascular events in post-MI patients. Pharmacologic therapies remain the cornerstone of management, but integrating dietary interventions may enhance long-term outcomes. Further large-scale, randomized studies across diverse populations are recommended to refine individualized treatment strategies and explore optimal combinations.
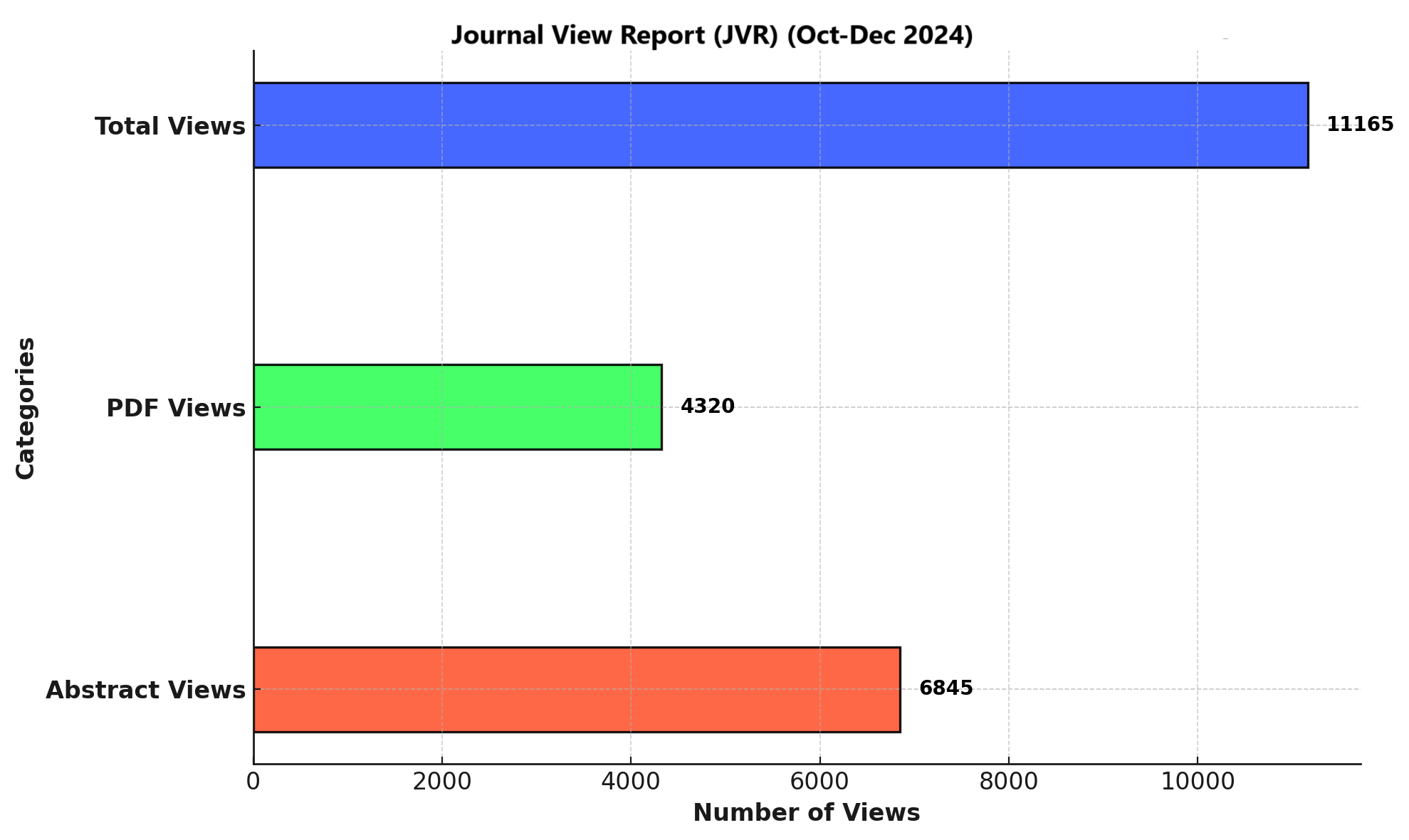
Downloads
Published
Issue
Section
License
Copyright (c) 2024 Muhammad Umer Khan, Ayesha Siddiqui, Mujtuba Siddiqui, Syeda Samia Shams, Aisha Alyassi, Burhan ali , Abdul Mateen Soomro, Muaz Shafique Ur Rehman, Ezaa Javed (Author)

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.