ROLE OF ELECTROLYTES AND INFLAMMATORY BIOMARKERS (CRP, ESR, PROCALCITONIN AND TLC) IN DEVELOPMENT OF NEONATAL SEPTICEMIA: A CROSS-SECTIONAL STUDY
DOI:
https://doi.org/10.71000/06kkq968Keywords:
C-Reactive Protein, Electrolyte Imbalance, Neonatal Sepsis, Procalcitonin, Sodium Disorders, Systemic Inflammation, Total Leukocyte CountAbstract
Background: Neonatal septicemia remains a major cause of morbidity and mortality worldwide, particularly in low- and middle-income countries, due to delayed diagnosis and nonspecific clinical presentation. The immature immune system of neonates limits their ability to mount an effective inflammatory response, making laboratory biomarkers essential for early detection. Inflammatory markers and electrolyte disturbances frequently accompany systemic infection, yet their combined diagnostic relevance in late-onset neonatal septicemia remains insufficiently explored in regional clinical settings.
Objective: To evaluate the diagnostic significance of key inflammatory biomarkers—C-reactive protein, procalcitonin, total leukocyte count, and erythrocyte sedimentation rate—and their relationship with electrolyte imbalances in neonates with late-onset septicemia.
Methods: A descriptive cross-sectional study was conducted in neonatal intensive care units of tertiary hospitals in Faisalabad, Pakistan. Fifty neonates were initially screened; thirty-five with early-onset sepsis were excluded. Fifteen neonates aged 3–28 days diagnosed with late-onset septicemia were included. Venous blood samples were analyzed for inflammatory biomarkers and serum electrolytes using standardized chemistry analyzers. Data were analyzed using SPSS, applying descriptive statistics and Pearson correlation analysis.
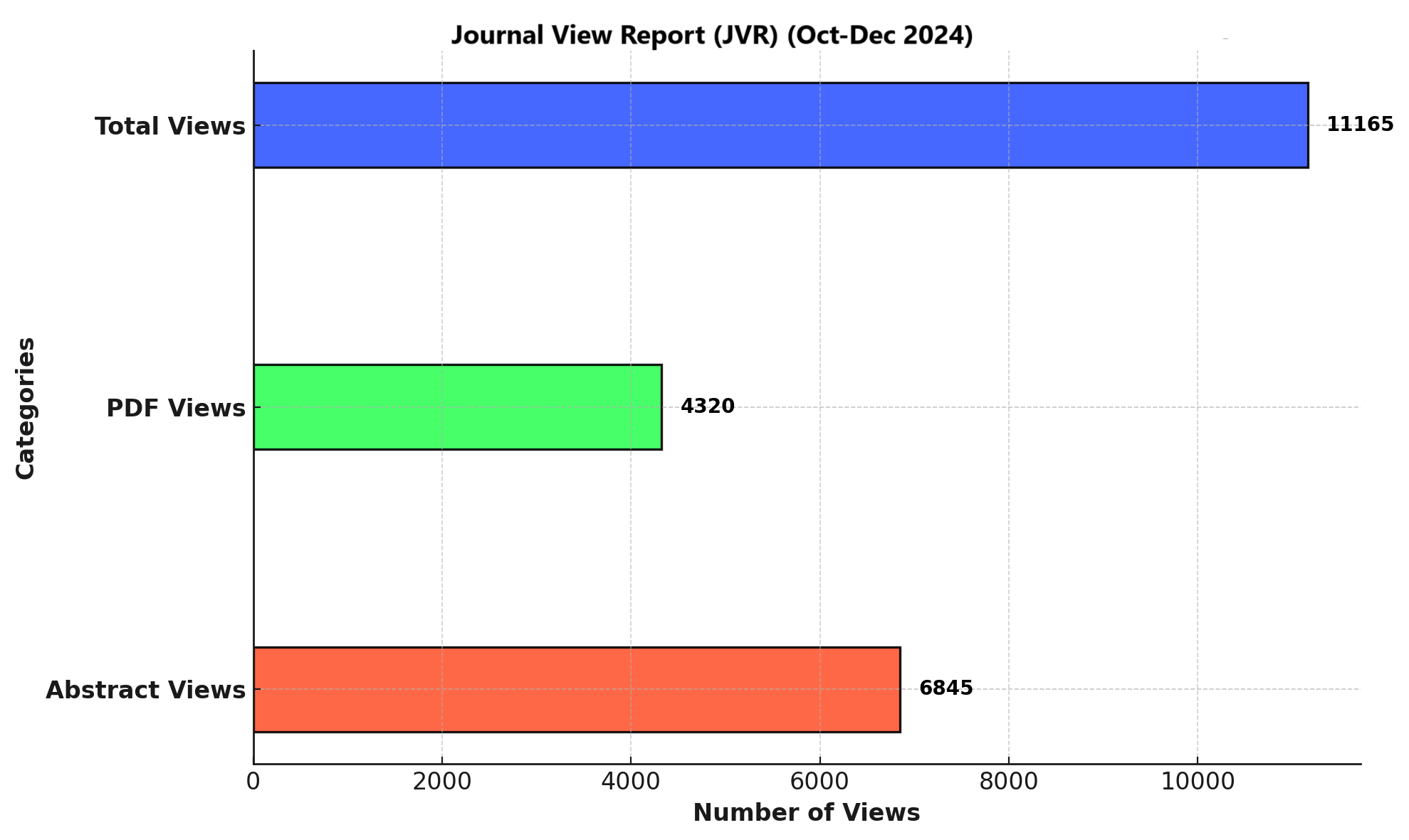
Results: Elevated C-reactive protein levels were observed in 12 neonates (80%), while procalcitonin was raised in 11 neonates (73.3%). Total leukocyte count was elevated in 7 cases (46.7%), and erythrocyte sedimentation rate in 5 cases (33.3%). Hyponatremia was present in 8 neonates (53.3%), hypochloremia in 6 (40.0%), and potassium imbalance in 7 (46.7%). A strong positive correlation was found between C-reactive protein and procalcitonin (r = 0.899), while moderate negative correlations were observed between inflammatory markers and sodium and chloride levels.
Conclusion: C-reactive protein and procalcitonin demonstrated superior diagnostic utility in late-onset neonatal septicemia. Electrolyte imbalances, particularly hyponatremia, were frequent and reflected systemic involvement. A combined assessment of inflammatory biomarkers and electrolytes may enhance early diagnosis and clinical management of neonatal sepsis.
References
Alende-Castro, V., Alonso-Sampedro, M., Fernández-Merino, C., Sánchez-Castro, J., Sopeña, B., Gude, F., & Gonzalez-Quintela, A. (2021). C-reactive protein versus erythrocyte sedimentation rate: implications among patients with No known inflammatory conditions. The Journal of the American Board of Family Medicine, 34(5), 974-983.
Anugu, N. R., & Khan, S. (2021). Comparing the diagnostic accuracy of procalcitonin and C- reactive protein in neonatal sepsis: a systematic review. Cureus, 13(11).
Boscarino, G., Romano, R., Iotti, C., Tegoni, F., Perrone, S., & Esposito, S. (2024). An overview of antibiotic therapy for early-and late-onset neonatal sepsis: Current strategies and future prospects. Antibiotics, 13(3), 250.
Cantey, J. B., & Lee, J. H. (2021). Biomarkers for the diagnosis of neonatal sepsis. Clinics in perinatology, 48(2), 215-227.
Celik, I. H., Hanna, M., Canpolat, F. E., & Pammi, M. (2022). Diagnosis of neonatal sepsis: the past, present and future. Pediatric research, 91(2), 337-350.
Chaudhuri, P. K., Ghosh, A., Sinha, V., Singh, B. K., Singh, M., Lugova, H., . . . Kumar, S. (2022). The role of C-reactive protein estimation in determining the duration of antibiotic therapy in neonatal sepsis. Cureus, 14(10).
Chen, J., Yasrebinia, S., Ghaedi, A., Khanzadeh, M., Quintin, S., Dagra, A., . . . Khanzadeh, S. (2023). Meta-analysis of the role of neutrophil to lymphocyte ratio in neonatal sepsis. BMC Infectious Diseases, 23(1), 837.
Coggins, S. A., & Glaser, K. (2022). Updates in late-onset sepsis: risk assessment, therapy, and outcomes. Neoreviews, 23(11), 738-755.
Eichberger, J., Resch, E., & Resch, B. (2022). Diagnosis of neonatal sepsis: the role of inflammatory markers. Frontiers in pediatrics, 10, 840288.
Flannery, D. D., Edwards, E. M., Coggins, S. A., Horbar, J. D., & Puopolo, K. M. (2022). Late- onset sepsis among very preterm infants. Pediatrics, 150(6), e2022058813.
Guo, L., Han, W., Su, Y., Wang, N., Chen, X., Ma, J., . . . Ren, C. (2023). Perinatal risk factors for neonatal early-onset sepsis: a meta-analysis of observational studies. The Journal of Maternal-Fetal & Neonatal Medicine, 36(2), 2259049.
Kaur, S., & Singh, K. (2021). Early-Onset Neonatal Sepsis: Role of C-Reactive Protein, Micro- ESR, and Gastric Aspirate for Polymorphs as Screening Markers. International journal of pediatrics, 2021(1), 1544553.
Khan, M. A., Alauddin, M., Amman, A., & Uddin, M. G. (2022). Outcome of Neonates with Septicaemia with Different Types of Electrolyte Abnormality. South Asian Res J Med Sci, 4(1), 9-12.
Khanum, A., Farhan, S., Arshad, S., Rashid, A., Kashif, A., Aslam, N., & Mazhar, N. (2021). Diagnostic Accuracy of Increased Total Leucocyte Count (TLC) and Decreased Absolute Neutrophil Count (ANC) for Diagnosis of Neonatal Sepsis Taking Culture Sensitivity as Gold Standard. Annals of PIMS-Shaheed Zulfiqar Ali Bhutto Medical University, 17(1), 08-11.
Kosmeri, C., Giapros, V., Serbis, A., & Baltogianni, M. (2024). Application of Advanced Molecular methods to study early-onset neonatal Sepsis. International Journal of Molecular Sciences, 25(4), 2258.
Mabbul, S., Ram, P. R., & Badabagni, R. (2024). Incidence, Risk Factors and Outcomes of Sodium Imbalance in Neonates: A Prospective Observational Study in a Neonatal Intensive Care Unit. Res. J. Med. Sci, 18, 119-123.
Mahmoud, H. A. H., Parekh, R., Dhandibhotla, S., Sai, T., Pradhan, A., Alugula, S., Abdin, Z. (2023). Insight into neonatal sepsis: an overview. Cureus, 15(9).
Masud, S., & Abudhair, I. (2025). Prevalence, Risk Factors, and Causes of Neonatal Sepsis: Insights from Hospitals in Tripoli-Libya. (AAJSR), 126-136.
Sands, K., Spiller, O. B., Thomson, K., Portal, E. A., Iregbu, K. C., & Walsh, T. R. (2022). Early- onset neonatal sepsis in low-and middle-income countries: current challenges and future opportunities. Infection and drug resistance, 933-946.
SB, J., Baskar, S., Fareed, M., Kumar, K. S., Mostafa, O. E., Bawazir, A., & AlQumaizi, K. I. (2025). Role of hematological parameters in the early detection of clinical cases for septicemia among neonates: A hospital-based study from Chennai, India. PloS one, 20(3), e0318802. Sharma, N., Singh, S., Thakur, B. R., Guleria, S., Pandit, P., & Guleria Sr, S. (2024).
Shoukry, L. R., Mohamed, A. N., Sharaf, A. E., & Osman, O. B. (2021). Diagnostic markers for early detection of neonatal sepsis. Journal of Scientific Research in Medical and Biological Sciences, 2(3), 13-26.
Sturrock, S., Sadoo, S., Nanyunja, C., & Le Doare, K. (2023). Improving the treatment of neonatal sepsis in resource-limited settings: gaps and recommendations. Research and reports in tropical medicine, 121-134.
Tum, F. C., Ngeranwa, J. J., Maiyoh, G. K., & Onyambu, F. G. (2025). Validity of procalcitonin and C-reactive protein as biomarkers in diagnosis of neonatal sepsis in a referral hospital, Kenya. Alexandria Journal of Medicine, 61(1), 60-66.
Yadav, P., & Yadav, S. K. (2022). Progress in diagnosis and treatment of neonatal sepsis: a review article. JNMA: Journal of the Nepal Medical Association, 60(247), 318.
Zieg, J., Ghose, S., & Raina, R. (2024). Electrolyte disorders related emergencies in children. BMC nephrology, 25(1), 282
Downloads
Published
Issue
Section
License
Copyright (c) 2025 Hafiz Muhammad Siddiq, Muhammad Najeeb Ullah, Dilawaiz Kabir, Sohail Sajid, Muhammad Muzammil, Muhammad Rashid, Rafia Anwer (Author)

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.